Regular exercise has long been recognized as a way to improve overall health and well-being. Exercise can reduce the risk of heart disease, stroke and obesity, among other ailments. However, what many people do not realise is that exercise can also have a positive impact on our eyes.
Studies have shown that regular exercise can reduce the risk of developing serious eye diseases that may lead to blindness. These diseases include diabetic retinopathy, glaucoma and macular degeneration, which are often linked to high cholesterol level, diabetes and high blood pressure. By reducing these risk factors, exercise can help preserve vision for a longer period.
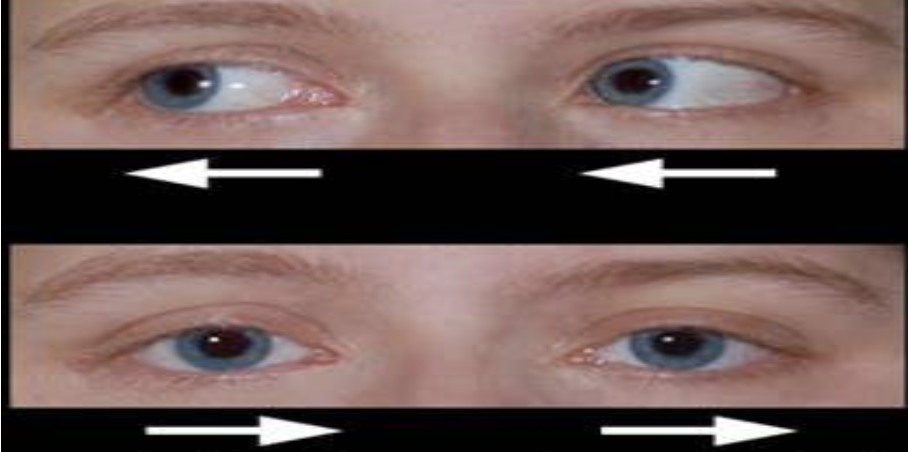
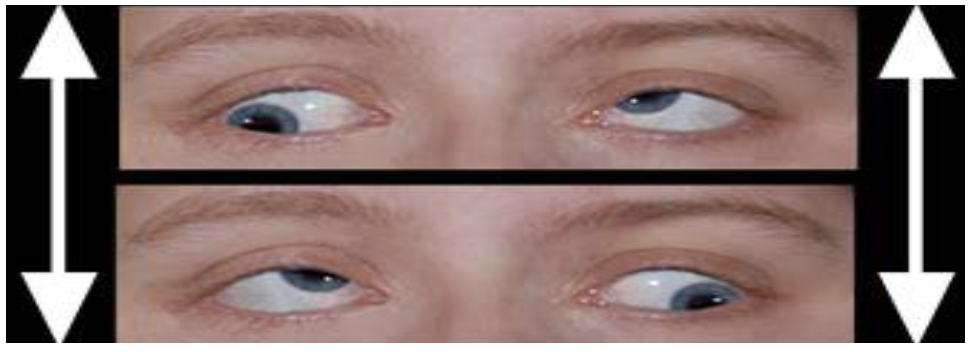
While no direct correlation has been found between exercise and glaucoma, research has shown that intraocular pressure is reduced after exercising. This is due to the acceleration of aqueous outflow, leading to lower intraocular pressure than usual. People who regularly exercise have a lower risk of developing glaucoma than those who do not. According to the American Academy of Ophthalmology, people who engage in moderate physical exercise are 25% less likely to develop glaucoma than those who are mostly inactive. However, caution should be exercised as certain positions and postures can exacerbate glaucoma, such as a head-stand.
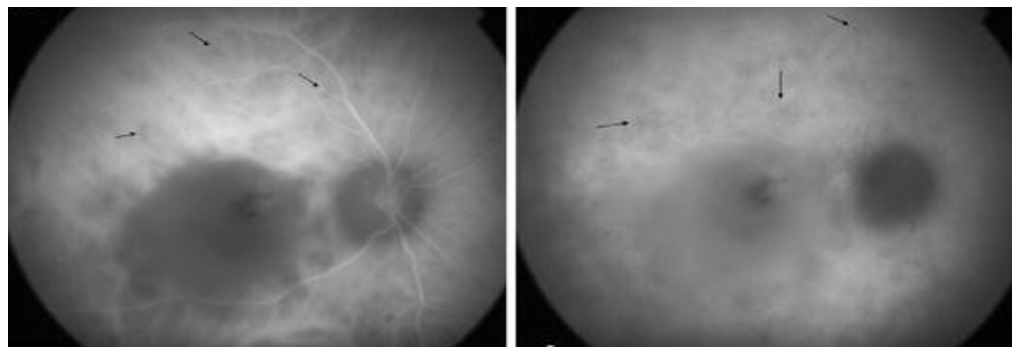
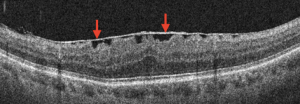
Age-related macular degeneration is a leading cause of severe vision loss worldwide in people over the age of 60. Although there is no direct link between exercise and macular degeneration, studies suggest that exercise can reduce the risk of developing the disease. This is because exercise can improve blood flow to the retina, which is essential for maintaining healthy vision.
In addition to reducing the risk of eye diseases, exercise can also improve energy levels, lower blood pressure and aid in weight loss. All these factors contribute to improved overall health and well-being. Regular exercise can promote a healthier lifestyle, leading to better rest for the body and improved quality of life.
In conclusion, exercise is beneficial not only for the body but also for the eyes. Regular exercise can significantly lower the risk of developing serious eye diseases. While exercise cannot single-handedly prevent or cure eye diseases, it can certainly help in your overall well-being. Additionally, it is crucial to get regular eye checks, as they can aid in the early detection of any eye disease. Don’t forget to visit our centre, OasisEye Specialists, where we provide comprehensive eye care services to help you maintain optimal eyesight.
Residents within Klang Valley in areas such as Cheras, Puchong, Shah Alam, Petaling Jaya, and Kepong can come visit our ophthalmologists to have their eyes examined at Nexus Bangsar South KL branch. Residents in Seremban 2, Senawang, Sendayan and Port Dickson can visit Dr Teh Wee Min at our Seremban branch. Residents in Johor Bahru, Skudai, Kulai, Iskandar Puteri, Senai, Tebrau, Batu Pahat, Kluang, Segamat can visit Dr Ling Kiet Phang or Dr Chan Choon Teng at our Johor Bahru branch. Residents in Perai, Bukit Mertajam, Butterworth, Penang island, Alor Setar, Kulim and Sungai Petani can visit Dato’ Dr Haslina at our Penang branch.